My Blog

Today I am delighted to welcome the release of an excellent report into services for new mothers and their babies. It is written by Sally Hogg at the NSPCC, entitled NSPCC Prevention in Mind – spotlight on perinatal mental illness REPORT FINAL
This report shows that we can, and we must, do more to prevent the harm caused by perinatal mental illness in England today. I shall ask you specific questions later on!
‘ It has shown the changes that are needed across the system to ensure that women with perinatal mental illnesses and their families get the right care, and it has shone a spotlight on the current gaps in services in England. It has included clear data on these gaps in services, but has also tried to bring to life what these problems actually mean for women themselves, and their lifelong impact on families.
… Government now needs to provide focussed and determined leadership to ensure that its commitments translate into reality for all families across the country.’
When my son was born, I spiralled down through various stages of postnatal depression until I needed hospital treatment for puerperal psychosis, an extreme form of the illness. I had begun to self-harm; my son was put on the at-risk register with Social Services; I attacked my father; my teaching career and relationships were in tatters. After walking the streets of a wet December night in my nightdress, I was admitted to a general psychiatric hospital ward for two months – without my baby. I was told there were no specialist Mother and Baby facilities available.
My baby was seven months old at the time and our sudden and forced separation could have added to the situation:
1. Abrupt breastfeeding can cause a worsening of depression due to the changes in hormones; the resulting pain and pressure of the breasts; the feeling of loss of something that was giving me a feeling of success. Seventeen years later I still feel robbed of the joy of breastfeeding.
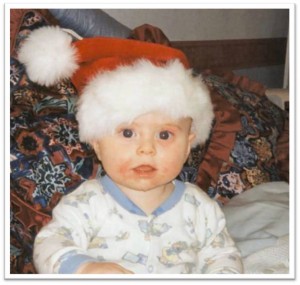
2. Postnatal illness can have a detrimental effect on the infant, resulting in years of psychological problems. This photo was taken on his first Christmas Eve, away from his Mum. The sorrowful look in his eyes and the eczema on his face (due to abrupt cessation of breastfeeding) are two key effects which continues to drive me to call for better services for all new mothers and their families.
It is very appropriate that NSPCC have produced this survey. At the most severe point of my illness, my poorly brain developed irrational and awful thoughts of harming my son. I had previously judged anyone who harmed a child extremely badly. Postnatal illness turned me into one of those ‘dreadful people’. Of course I would never condone anyone who harms a child – what I can say is that in some cases now I can understand it. For a relatively brief and very scary time in my life, it was something I potentially could have done. That is one of the many reasons we must make the services better. I wish I had been placed in a Mother and Baby Unit with my son so that the bonding and success I had with breastfeeding could have continued (under supervision) and our relationship rebuilt. Severing that bond at that crucial time could have pushed me to suicide due to the extreme sense of failure and hopelessness that I felt.
Electro-convulsive therapy (ECT) was the treatment that put me back on the road to recovery, along with medication, counselling and the support of family and friends. I am eternally grateful that I did get better. On reflection I recognise that the pain that we all went through as a family, could have been lessened by better services and my behaviour.
Yes, I had a network of services around me before my ‘breakdown’. It seemed that they did not connect and I slipped through the net. I also had a role to play in my ‘illness’. The guilt and shame I perceived as being ‘mentally ill’ drove me to hiding many of my true emotions at the time. So many times I put the mask of “I’m fine” on when I wasn’t. I strongly encourage sufferers to be candid. Be as honest as you would if you had a physical pain. Perhaps if I had, I might not have become so poorly. One perinatal psychiatrist also said that I should have been ‘picked up earlier’ by a specialist, also reducing the severity of the illness. In the long run, this would have saved the NHS thousands of pounds, immaterial of the human costs. Later on my marriage failed – mainly due to the longer term effects of the illness on us both.
I shared my story in ‘Eyes without Sparkle – a journey through postnatal illness’ (Radcliffe, 2005) because I wanted to show how a life can unravel through having a baby. Most importantly, I wanted to show how you CAN get well. I am humbled to say that I know of at least four ladies who are alive today because my story gave them hope at a time when they considered suicide.
I gave up my teaching job in 2005 to pursue my purpose in helping make early parenthood happier for others. I have travelled the world as a result. I have been privileges to learn much about perinatal mental health and am currently working on my next book which will be on ‘Contemplating Pregnancy after Postnatal Illness.’
Although my son is now 17, so many others have shared their stories with me and continue to do so. Almost on a daily basis, a family share their pain with me over postnatal illness. Due to this I am able to be ‘every woman’s advocate of postnatal illness’ as I was recently described. My heart goes out to every family who give me the privilege of sharing their story with me. Many have been inspired to set up support groups or do something to help others. Why? Perhaps because, like me, they felt their suffering could have been reduced. Perhaps they have witnessed others who have had a well and happy early motherhood experience and forever feel that it was stolen for them, so they want to help others.
As a teacher my passion remains for enabling others to learn and I do this by speaking to as many audiences as possible. My current keynote address is aimed specifically at postnatal depression and the effects on breastfeeding. I commend the NSPCC report for stressing the need for more education of health professionals, especially GPs. Many mothers tell me of their despair at being ‘fobbed off’ or simply not being giving information they need. I feel so sorry when healthcare professionals tell me of their huge concerns around the lack of continuity of care; the cutting of basic services like antenatal classes and health visiting. There are some excellent and dedicated team members out there who are doing their best against all current odds.
I believe that we all have a role to play in improving services:
1. All of society to have the belief that postnatal depression is an illness – that sufferers need the emotional and practical support as they would for any physical illness. Next time you are at your GPs, ask them if they have seen the report and had training.
2. As a sufferer, work hard at ignoring the stigma and focus on accepting that you are unwell. Be candid and honest when you are asked how you feel and seek out the best services.
3. If you have been affected by postnatal illness in any way, tell your story! Share the impact it has had on you as a child, mother, father, friend or colleague. The more weight we can put behind it, the better. By all means, send them to me and I will collate them.
4. As a close loved-one or friend of a sufferer, be there for them. There is no need to ‘fix’ the situation or be judgemental. Sometimes a listening ear, a spot of shopping or doing a pile of ironing can be huge ways to help.
5. As a health professional, if you are not trained in perinatal mental health – ask for it! If you know you need more services – make a noise! Go to your commissioners and show them the NSPCC report and also the Commissioners Guide for Perinatal Services.
6. Where there are the services and funding, ensure that they are the best they can be.
7. Share the details of the NSPCC report via your contacts – include LinkedIn, Twitter, Facebook. Who is your MP? Point it out to them. The Royal College of Obstetricians and Gynaecologists have commented here on the report.
Let’s finally get some action in this area.
Now, what will you do to help?
Elaine