My Blog
‘Improving the quality of perinatal mental health services’ is at the heart of my purpose in life. Yesterday I was privileged to chair and speak at a conference with that title. This is the fourth that I have been asked to do organised by Healthcare Conferences UK. It was the best so far!
From the arrival of the first delegate, who was new to this area and wants to make a real difference to the lives of new mothers, it was clear that the room was full of equally passionate people. As I asked everyone to introduce themselves I was delighted at how many used the term ‘perinatal’ in their roles. Five years ago that was a word that was hardly used and maternal mental health tended to be clustered under ‘postnatal depression’ in services. The change of title implies that we are now seeing a much needed focus on the diversity of conditions that can affect families in the antenatal and postnatal period.
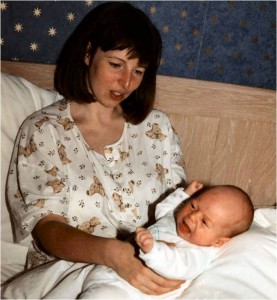
I began the day by sharing my story and those of some other mothers. I shocked myself with my emotional response as I described the December night I went walking in my nightie. It rang so close to the terrible death of Charlotte Bevan and her baby daughter last week and I had to pause to gather myself together. I do not like to show such emotion on the platform. I could not help it this time. Yet that is why we were there – we want and need to prevent these tragedies. This was me as I was spiralling down into puerperal psychosis.
Nigel Perks from Lewisham and Greenwich NHS trust spoke next. Their Perinatal Mental Service has just been awarded a prize from the All-Party Parliamentary Group on Maternity (APPGM).He stressed the need for ‘identification through communication’ and how professionals need to be aware of picking up the signals to access the mental state of a new parent.
Next we heard from Peter Thompson from the Royal College of Psychiatrists. He shared with us the standards that they use to ensure quality of perinatal mental services in specialist Mother and baby units and increasingly in community services. It is possible for interested people to join their forums. I mentioned the story of Grace Sharrock who describes her use of a MBU as a teenage mother with psychosis in her book, ‘Saving Grace – a journey through postnatal illness’. Yet again we hear of another unit closing down – this time at Eastbourne. There is a campaign to get the one reopened in Wales.
https://you.38degrees.org.uk/petitions/no-mother-and-baby-unit-in-wales-perinatal-mental-health
Why, oh why does this keep happening? Can you imagine the uproar if a cardiac unit closed? These aren’t just about inpatient beds – they can be centres of excellence that reach out to the communities they serve.
Mark Williams then spoke passionately about his story and his drive to ensure that fathers are a lso included in perinatal mental health services. I loved his statements that ‘prevention is the aim before the crisis point is reached’ and that living with a partner who has postnatal depression is like ‘living with a stranger’. The new website will be www.fathersreachingout@gmail.com
After lunch we were fascinated by a presentation by the inspiring Jane Hanley on ‘Listening to mother wherever they are’. Jane had been president of the Marce Society for the conference I attended back in September. I am sure I am not the only one who could have listened to her all day! Jane gave delegates the encouragement to listen to those women who are possibly finding the cultural aspects of childbirth difficult, especially in relation to mental health and especially if they are unable to speak English. She described some of the beliefs and rites of passage attached to motherhood, e.g. churching of women and about Jinn, a spirit in Muslim mythology. She asked delegates to consider their own thoughts and feelings about communicating with a mother who cannot speak English or perhaps is reluctant to speak freely of her mental health due to cultural aspects. She suggested that they found out what local sources of support there are; learn some key phrases in their language using Google translate and find out what their cultural beliefs and traditions are around childbirth.
http://www.health.qld.gov.au/multicultural/support_tools/14MCSR-pregnancy.pdf is where you can find a guide for some cultural dimensions of pregnancy, birth and postnatal care. You may find some cultural guides via UKTI – although these are based for business, there are some indicators around customs, e.g. http://www.china.doingbusinessguide.co.uk/.
I then shared some of the main resources that I have found useful around perinatal mental health.
The day concluded with another passionate and inspiring presentation by Pauline McPartland from PSS in Liverpool. She described their great Parent and Baby Wellness Service and showed a little of their DVD.
Apparently the feedback on the day was very good. I do hope that delegates left feeling informed and inspired.
As I left, we secured the next one for May 19th 2015. Thank you Healthcare Conferences for enabling this great day and I look forward to the next. Book here. Thank you to the other speakers and delegates for sharing the day together.
Whilst I was in London I took the opportunity to meet my publisher. My second book is due to be completed at the end of January looking to publication in June/July 2015. Watch this space!
Have a great weekend,
Elaine